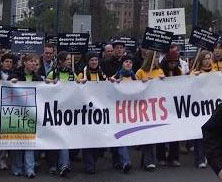
In Washington, DC, no protections exist for unborn children and for their mothers from the harms that abortion inflicts. This week, Congress will have a chance to remedy that. The House of Representatives will hold a vote on the H.R. 3803: the District of Columbia Pain-Capable Unborn Child Protection Act. At stake, the long-term welfare of women, girls and their unborn children.
 If passed, this bill will prohibit abortions in the District of Columbia after 20-weeks’ gestation. And H.R. 3803 not only protects the unborn child, whom the medical community has acknowledged can feel pain at least by 20-weeks’ gestation, but also protects the mother from heightened physical and psychological risks from abortion. Complications from such late-term procedures are detailed in a growing body of medical data and cause for great concern.
If passed, this bill will prohibit abortions in the District of Columbia after 20-weeks’ gestation. And H.R. 3803 not only protects the unborn child, whom the medical community has acknowledged can feel pain at least by 20-weeks’ gestation, but also protects the mother from heightened physical and psychological risks from abortion. Complications from such late-term procedures are detailed in a growing body of medical data and cause for great concern.
Medical evidence reveals that abortion, and late-term abortion in particular, creates significant health risks for women including uterine perforation, uterine scarring, cervical perforation, infection, bleeding, hemorrhage, blood clots, incomplete abortion, pelvic inflammatory disease, metabolic disorder, free fluid in the abdomen, organ damage, and psychological complications such as depression, anxiety, and sleeping disorders.
These risks to women’s health increase as pregnancy progresses.[i] The physical complication rate from abortion is at least 50% when the abortion is performed during, or after, the second trimester (i.e., 13 weeks and beyond). [ii]
Research also indicates that late-term abortions carry an elevated mental health risk.
A 2010 study comparing the mental health of women undergoing early versus late-term abortions found that women who underwent later abortions (13 weeks or beyond) reported “more disturbing dreams, more frequent reliving of the abortion, and more trouble falling asleep.”[iii] The same study ultimately concluded that women who wait until the second or third trimester before undergoing an abortion have an increased risk of the “unwelcome re-experienc[ing] of the abortion procedure”—reminiscent of post-traumatic stress disorder—that may require professional counseling.[iv]
Notably, the risk of death for the mother is significantly higher when abortion is performed during later stages of pregnancy. A study of national data in the U.S. on abortion-related mortality from 1988-1997 found that at 13-15 weeks of gestation, the rate of abortion-related mortality was 14.7 deaths per 100,000 abortions; at 16-20 weeks, the rate rose to 29.5 deaths per 100,000 abortions; and at or after 21 weeks, the rate reached 76.6 deaths per 100,000 abortions.[v] This study clearly shows that the later in pregnancy the abortion occurs, the greater the risk of death for the woman.
Not only do women suffer greater risk of physical and psychological injuries from later abortions, their very lives are at risk as well. This should serve as impetus for Congress to act and pass the D.C. Pain-Capable Unborn Child Protection Act, prohibiting abortion after 20-weeks’ gestation in the District of Columbia. The women of our Nation’s Capital deserve it.
CLICK LIKE IF YOU’RE PRO-LIFE!
[i] Several large scale studies reveal that abortions after the first trimester (144,000 performed annually) pose more serious risks to women’s physical health than first trimester abortions. S. V. Gaufberg, “Abortion complications,” 2008, https://emedicine.medscape.com/article/795001-overview (last visited May 31, 2012.) L. A. Bartlett, C. J. Berg, H. B. Shulman et al., “Risk factors for legal induced abortion-related mortality in the United States,” Obstetrics and Gynecology, vol. 103, no. 4, pp. 729–737, 2004.
[ii] See Slava V. Gaufberg, Abortion, Complications, eMedicine, Feb. 5, 2010, available at https://emedicine.medscape.com/article/795001-overview#a0199 (last visited July 19, 2012).
[iii] Coleman, Coyle & Rue, Late-Term Elective Abortion and Susceptibility to Posttraumatic Stress Symptoms, 2010 Journal of Pregnancy 1, 7.
[iv] Id at 8.
[v] Bartlett, supra







